Are you ready to uncover the mysterious impact that How Psoriasis Affects the Body?
Brace yourself for a transformative journey as we delve into the depths of this enigmatic condition.
Psoriasis, a silent warrior that affects millions worldwide, goes far beyond its visible symptoms, leaving an indelible mark on both your physical and emotional well-being.
In this compelling blog post, we will unveil the hidden secrets of how psoriasis affects the body while empowering you with seven transformative ways to take charge of your health.
Get ready to challenge conventional perceptions, embrace your uniqueness, and embark on a path to holistic empowerment. It’s time to unveil the power that lies within your skin and rewrite the story of psoriasis. Are you prepared to explore the extraordinary?
Then let’s dive in!
What is Psoriasis?
Psoriasis, a non-contagious chronic skin condition, is characterized by an intricate interplay between the immune system and the skin. It occurs when the immune system becomes overactive, mistakenly attacking healthy skin cells as if they were harmful invaders.
This immune system malfunction triggers an accelerated production of skin cells, causing them to rapidly accumulate on the surface of the skin.
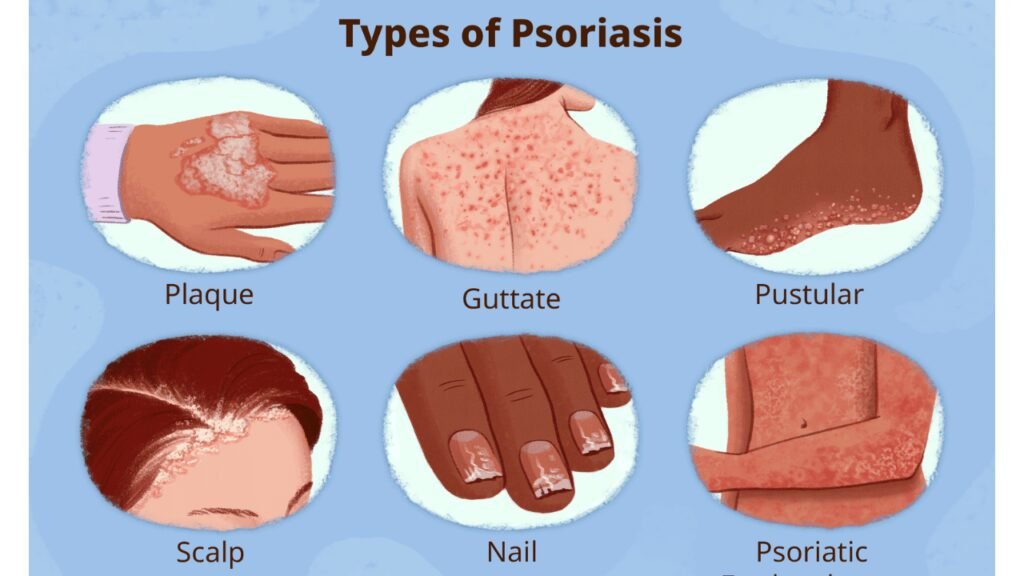
The hallmark of psoriasis is the formation of raised, red patches of skin called plaques. These plaques are often covered with silvery-white scales, giving them a distinct appearance.
While psoriasis can affect any part of the body, it most commonly occurs on the elbows, knees, scalp, and lower back.
Underneath the surface, psoriasis goes beyond a mere aesthetic concern. The rapid growth of skin cells and the subsequent accumulation on the skin’s surface can lead to discomfort, itchiness, and pain.
In severe cases, psoriasis can interfere with everyday activities and impact a person’s quality of life.
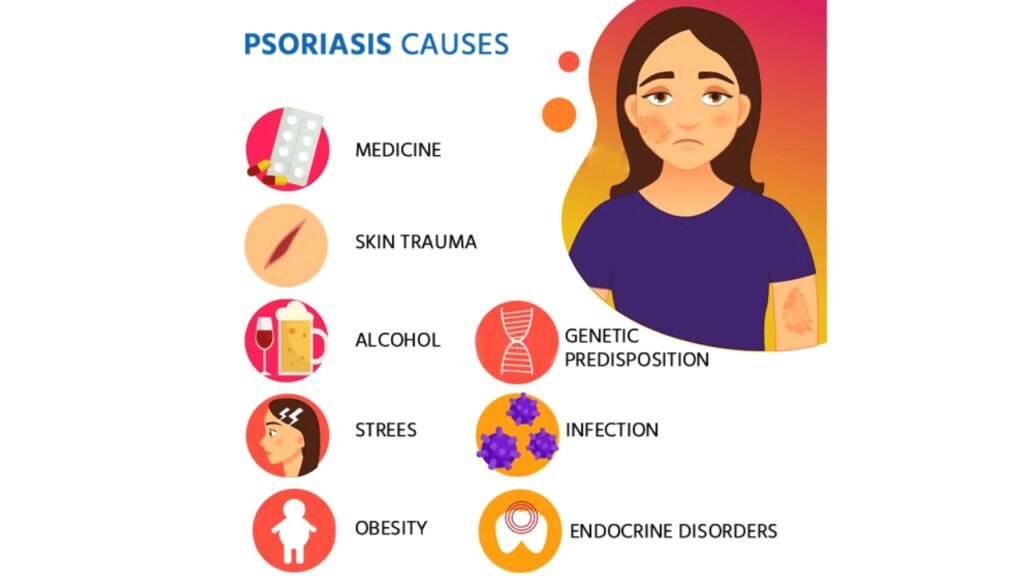
The Causes of Psoriasis
While the exact cause of psoriasis remains unknown, several factors are believed to contribute to its development.
Genetic predisposition, immune system dysfunction, environmental triggers, and certain lifestyle factors can all play a role in the onset and progression of psoriasis.
Impact of Psoriasis on the Body
Psoriasis extends beyond the visible symptoms on the skin. It can affect various aspects of the body, leading to physical discomfort and emotional challenges.
Skin Inflammation and Flaking
One of the primary effects of psoriasis is the inflammation of the skin, resulting in redness, itching, and flaking.
The constant shedding of skin cells can cause embarrassment and self-consciousness, impacting an individual’s self-esteem.
Joint Pain and Swelling
Psoriatic arthritis, a common complication of psoriasis, affects the joints, causing pain, stiffness, and swelling.
This condition can significantly impact a person’s mobility and overall quality of life.
Emotional and Psychological Effects
Living with psoriasis can have a profound impact on a person’s mental well-being. The visible symptoms, social stigmatization, and the chronic nature of the condition can lead to feelings of depression, anxiety, and isolation.
Association with Other Health Conditions
Psoriasis is not just a skin disorder; it is also associated with other health conditions. Research has found links between psoriasis and various comorbidities, such as cardiovascular disease, diabetes, obesity, and certain autoimmune disorders.
The underlying inflammation and immune dysregulation in psoriasis can contribute to the development or worsening of these conditions.
It is crucial for individuals with psoriasis to be aware of these associations and work closely with healthcare professionals to manage their overall health.
Diagnosing Psoriasis
To accurately diagnose psoriasis, healthcare professionals typically conduct a thorough examination of the skin, review the patient’s medical history, and may perform additional tests if necessary.
It is important to consult a dermatologist or a qualified healthcare provider for an accurate diagnosis and appropriate treatment plan.
Management and Treatment Options
While there is currently no cure for psoriasis, there are several management and treatment options available to alleviate symptoms and improve quality of life.
Topical Treatments
Topical treatments, such as corticosteroids, moisturizers, retinoids, and salicylic acid, are often the first line of defense for mild to moderate psoriasis. These medications help reduce inflammation, remove scales, and moisturize the affected skin.
Systemic Medications
For more severe cases of psoriasis, systemic medications may be prescribed. These medications, including methotrexate, cyclosporine, and biologics, work by suppressing the immune system or targeting specific inflammatory pathways. They require careful monitoring and may have potential side effects, so regular follow-ups with a healthcare provider are essential.
Phototherapy
Phototherapy involves exposing the skin to controlled doses of ultraviolet light. This treatment option can help slow down excessive skin cell production and reduce inflammation. Phototherapy can be administered in various forms, such as narrowband UVB, PUVA (psoralen plus ultraviolet A), or targeted phototherapy.
Lifestyle Changes and Self-Care
In addition to medical treatments, certain lifestyle changes and self-care practices can help manage psoriasis symptoms. These include maintaining a healthy diet, managing stress levels, avoiding triggers, practicing good skincare habits, and incorporating regular exercise into daily routines. It is important to work with healthcare professionals to develop a personalized management plan that suits individual needs.
Coping Strategies and Support
Living with psoriasis can be challenging, both physically and emotionally. However, there are coping strategies and support systems available to help individuals navigate their psoriasis journey.
Dealing with the Emotional Impact
Coping with the emotional impact of psoriasis is essential for overall well-being. It is important to address any feelings of embarrassment, self-consciousness, or depression that may arise from living with a visible chronic condition.
Seeking support from loved ones, joining support groups, or consulting with mental health professionals can provide valuable emotional support.
Seeking Professional Help
Working closely with healthcare professionals, such as dermatologists and rheumatologists, is crucial for effective management of psoriasis. These specialists can provide accurate diagnosis, recommend appropriate treatment options, and monitor the progress of the condition.
Regular check-ups and open communication with healthcare providers can help individuals stay on top of their psoriasis management.
Joining Support Groups
Joining support groups or online communities dedicated to psoriasis can provide a sense of belonging and understanding. Interacting with others who share similar experiences can offer valuable insights, tips, and emotional support.
These communities can also provide a platform to discuss challenges, share success stories, and exchange information on the latest research and treatments.
Conclusion
In conclusion, the journey of understanding how psoriasis affects the body has taken us through a labyrinth of insights, unveiling the intricate interplay between our immune system, genetics, environment, and lifestyle factors. We have discovered that psoriasis extends beyond its visible manifestations, reaching deep into our physical and emotional well-being.
However, this knowledge is not meant to overwhelm or discourage us. Instead, it is an invitation to embark on a transformative path of empowerment. By embracing our uniqueness, challenging conventional perceptions, and adopting a holistic approach to psoriasis management, we can reclaim control over our health and well-being.
Remember, psoriasis does not define who we are. It is a part of our journey, but it does not diminish our worth or potential. Let us view our psoriasis as a catalyst for growth, resilience, and self-compassion. Let it fuel our determination to lead fulfilling lives, pursue our dreams, and cultivate meaningful connections.
As we conclude this exploration, let us embrace the power within our skin, recognizing that we are more than our conditions. Let us unite in support, empathy, and understanding, shattering stigmas and fostering a society that embraces diversity and celebrates the beauty of every individual.
So, stand tall, my friend, for you possess the strength to navigate the challenges that psoriasis may bring. Embrace the seven transformative ways to empower your health, and let them guide you towards a life filled with self-acceptance, resilience, and hope.
Together, let us embark on this journey of empowerment, breaking barriers, and nurturing a community where psoriasis is not an obstacle, but a catalyst for personal growth and compassion. Remember, you are not alone, and your story has the power to inspire and uplift others.
As we part ways, may this newfound understanding and resilience propel you towards a brighter future, where psoriasis becomes a chapter in your journey, but not the defining story. Embrace your strength, nurture your well-being, and continue to shine as a beacon of inspiration.
You are more than psoriasis. You are extraordinary.